HEALTHspital 6.0
1 JUNE 2016 [ Major Revision # 1 ] [ Update # 2 of Major Revision # 1 10 APRIL 2019 – REASON : New Website / Aquarian ]
12 MacKinnon Place
East Lyme
Connecticut 06333 – 1533
USA
HEALTHspital © 6.0 + – Original Vision Expressed in THE FUTURIST MARCH – APRIL 2011
– Concept and neologism originated 1998
FRANK W MALETZ MD FACS
Web Analogy :
1.0 Place / Address
2.0 Search eg Google
3.0 Individuated / Preferences eg Amazon
4.0 Expert System Links eg BEST MOM s ( Moments Of Magnificence ) and POP s
( Pockets Of Perfection )
5.0 WELLBEINGULARITY ©
6.0 EMERGENCE / EMERGENT Phenomena – Washington DC World Future Society
50 th Birthday Convening / Summer 2016
+…………… TBD
PREMISE / PROLOGUE / RIGHT QUESTIONS :
- Are Health , Wellness , Well Being , and Healthful Productivity a COMMONS ( CPR – Common Pool Resource – as defined by Elinor Ostrom ) ? AND , if re – visioned thus , can a bold , abundant , new model be re conceptualized of nested micro – eco – logical systems , integrally interconnected and interrelated holistically ?
MY EMPHATIC ANSWER IS YES !
- Are Health , Wellness , and Well Being , by agreed definition and as conceptualized , the same as to general understanding , meaning , and for practical applications ( FWM – see essay ) ? I suggest NO .
- Are Health , Wellness , and Well Being human rights – accessible to all and equitable for all inhabitants of Spaceship Earth ? I suggest YES and NOT YET x2 .
Our NEXT step :
To co create , co design , AND deeply co llaborate in the actualization / realitization of –
A TRUE HEALTHCARE COMMON s AND PRACTICE OF GLOBAL HEALTH , WELLNESS , AND WELL BEING , CARE AND CARING + – CO OPERATIVE s BASED IN LOCAL COMMUNITIES – HEALTHspital s –
A NOVEL CO PRODUCTIVE VALUE ENHANCING AND GAIAN ENNOBLING HEcoSystem !
OUTLINE
- Prologue
- A Look Back : Goals / Hopes / Aspirations
1) IHI ( 2007 ) Triple Aims ( Institute of Healthcare Improvement )
– Improve the health of the defined population
– Enhance the patient care experience ( including quality , access , and
reliability )
– Reduce , or , at least , control , the per capita cost of care
2) IOM ( Institute Of Medicine ) : THE CHASM – A NEW HEALTH CARE SYSTEM
FOR THE 21st CENTURY
3) RANKING s AND EXPENDITURES – US comparisons
- Known Knowns
- Hospitals Today
- Pillars
1) THE HILL OF RIGHTS
2) LEAN / TPS / LOWN / WASTE , FRAUD , ABUSE / UNNECESSARY
REDUNDANCY AND DUPLICATION
3) CHRONIC AND COMPLICATED – Fragmentation
4) END OF LIFE
5) PRE s PRO s RE s CO s
- Community Integration ————> Scale eg MetaCommunity Of Communities ©
- Bumps and Barriers
1) TRADITIONS
2) CONVENTIONS
3) SUNK COST s
- My Current Steps :
1) CEO – STAFF – HOSPITAL
2) WEBSITE
3) WRITINGS
4) UNIVERSITY / ACADEMIA
5) “ SYSTEM “ PARTNERS
6) AFFILIATIONS
7) VENTURE CAPITALISTS ———–> ADVENTURE CONTRIBUTIONISTS ©
- Preparing for the NEXT world of Planetary Health which does not exist – YET
1) GEMS : Gedanken Experimental Mind Spaciousness
2) WEAK SIGNAL Identification AND Augmentation / Amplification – L Audible
3) SIGNAL / NOISE SIFTER AND SORTER
4) CAS ( Complex Adaptive System s ) ———–> Co Creative Adeptive Eco Logical
Eco System s
5) EMERGENCE : Co Facilitated Nudging——-> R – Evolution ( Thaler / Sunstein )
6) MATHEMATICAL MODELING :
– Bob Emiliani – LEAN
– Michael Porter – Harvard Business School
– University of Minnesota – Pesut / Potter / O’ Day / Anderson
– Plexus Institute – Easton
– Y Vodovotz Phd – Computational Modeling
7) Communities Of The Future – COTF 1.0 – Smyre / Richardson / Maletz /
Arrington / Baldwin / Bost / Damicis / Fleener / O ‘ Day / Bourcier / el al
8) DEMOCRACY COLLABORATIVE – Alperovitz / Speth / Howard
Is the practice and delivery of “ health “ care as presently offered to “ carees ” in the US and globally so broken , dislocated , disarticulated , fractured , and fragmented that it cannot be repaired , remediated , rejuvenated , reformed , or reorganized ? Should we tear down existing models with their respective infra – and super – structural elements and components and start anew , do – over , from scratch ? As a practicing Orthopaedic surgeon I have spent an entire career in the domain of “ internal fixation “ and re locating – helping to heal the fragments back into wholes , dys – ease back into optimal function and functionalities .
I am by nature NOT a Schumpeterian , and my response to the suggestion for total annihilation / decimation , the phoenix phenomenon , and “ creative destruction “ is an unequivocal NO . But co creative Re VISIONING is imperative . There are no exemplars , no perfect , perfected , or perfecting systems of integrated health and wellness currently on this planet . There are micro – and macro – systems and , definitely , many MOM s and POP s to be celebrated and scaled . There is no ECOSYSTEM , fully integrated in any locale , and , certainly , no global HEcoSystem approach to this vital practice ( Fritjof Capra / Pier Luisi – THE SYSTEMS VIEW OF LIFE ) .
Care is not “ delivered “ – like delivering a pizza – it is an ongoing “ practice “ . While “ practice makes perfect “ is asymptotic as an “ end “ , evolutionary events have no END , no end point . “ Perfection “ , therefore , is aspirational and motivational . And the path , the purposeful journey , toward perfection and its relentless pursuit is worth every incremental step AND monumental leap with momentum and robust diligence .
What does an Eco Logical Eco Systemic approach actually mean ? An ecosystem , more than the present ubiquitous buzzword “ system “ is a natural system , with known and identifiable inputs and outputs , precise and defined ingredients , constituents , and resources , and with integrated and sustainable feedback and feedforward loops which abide continual learning and iterative improvements within networked cycles and epicycles . There are controls and balances , checks and constraints . But more importantly , ecosystems allow for emergent phenomena to which adaptivity , adjustability , and accommodation can be evolved . AND most impressively , at their best , adeptability , novelty , and paradigm – launching breakwiths will be R – Evolved toward NEXT betters and bests . Perturbations ( natural and [ hu ] – man made ) and scarcities will impact , but a true ecosystem will respond with resonance damping re balancing and proportionate mechanisms relatively seamlessly and usually toward harmony . By this discussion it is crystal and with absolute assurance that we do not have YET a HEcoSystem in health and wellness practice !
Could one be conceived and co crafted ?
What are the essential l ingredients , components , players , species ( keystone and rivet ) for the totipotential EcoSystem ? :
-patients ( CAREES )
-providers ( CARORS )
-payors
–insurance / insurers
–individuals / families
–employers
–governments
-pharmaceuticals
–trade
–generic
-device manufacturers
-research and development
–corporate
–university
–private
-attorneys / legal
-supply chains
–distribution chains of goods / services
–marketing / sales
-informatics and analytics
Oh , what a tangled , networked web we have already woven. Add to this complicated list , needs ( met and unmet ) and wants , sunk costs and current investment portfolios , reputations based on predictions and projections ( whole academic and bureaucratic hierarchical careers – egosystems © ) . The terms GARGANTUAN / BEHEMOTH are not imprecise adjectival appellations to apply to the chaos / disarray / disorder at present . How do we move such a colossus? Again , a true EcoSystem utilizes its BEST s and adapts to change , relishes complexity and grander scale . If we alchemize human ingenuity to this fertile mix , an “ enginuity © “ is co created which will leverage , optimalize , and launch adeptively , reliably , this entity proposed herein .
We begin from a position of great strength and existing , triumphant accomplishments . Expertise is abundant at universities , research labs , and startups . In the US , our predominantly free – market economy , if unencumbered , ignites invention and innovation ( constructive AND disruptive – I make no distinction – innovation IS innovation ) – any encumbrances and unnecessary , layered complicatifications must be vigilantly monitored and streamlined or eliminated . Safety is assisted by oversight bodies like the US Food and Drug Administration , The Joint Commission ( TJC ) , accreditation and state mandated programs and agencies . Chaos and duplication reign in this arena as well . Research grants and public access to those projects are prioritized by the National Institutes of Health . Private foundations in the space , notables include the Robert Wood Johnson Foundation , Melinda and Bill Gates , and various institutes and think tanks , as exemplified by Plexus Institute , populate the external milieu with great pro fund ity and foresight . Social networking tools ( wikis , search engines , Google , Facebook , Doximity , LinkedIn ) proliferate awaiting Big Data coordination and convergence platforms into the health care and well – being space .
So , how are we doing thus far ? There have been some major signposts . The Institute of Medicine published CROSSING THE QUALITY CHASM : A NEW HEALTH SYSTEM FOR THE 21 ST CENTURY in March 2001.
The following recommendations were highlighted:
– Redesign care processes
-Make effective use of information technology
-Develop effective teams
-Coordinate care across patient conditions , services , and settings
-Use performance and outcome measurement for CQI and accountability
The next blueprint was promulgated by the esteemed Institute For Healthcare Improvement named THE TRIPLE AIMS.
– Improve the health of defined populations
-Enhance the patient care experience ( including quality , access , reliability )
– Reduce , or at least control , the per capita cost of care
Also , concurrent with these major templates , the Harvard Business School think tank has substantive tomes on CONSUMER – DRIVEN CURE ( Regina Herzlinger ) , THE STRATEGY THAT WILL FIX HEALTH CARE ( Michael E Porter and Thomas H Lee MD ) , AND REDEFINING HEALTHCARE ( Michael E Porter and Elizabeth Olmsted Teisberg ) . The word “ value “ has been similarly popularized , along with “ system “ in myriad publications . That term VALUE is defined as :
VALUE = Quality / Cost
But , these are all , I proffer , incremental , partial , siloed , patchwork , further fragmented , evolutionary , surface , micro – improvements , but improvements nonetheless , to the existing order , hypotheses , models , and designs . While I never disparage forward movement , lessons learned , and momentum , the facts still unequivocally show that each and every one of the above listed ideas or panels of ideas have failed in every measure of health quality and cost stabilization to move the needle , especially in the US . We are on track to expend $3 TRILLION per year / 20% of our GDP on “ healthcare “ and statistically have a worsened prognosis regarding a substantive return on that investment . We are seeing longevity ( a crude proxy for Health ) decline for the first time in over a Century in the US . Who is at fault in the omnipresent finger pointing blame game : patients ( demands and expectations ) , providers ( overtreatment , overtesting to reduce malpractice perceived risk , overdiagnosis ) , insurers ( playing doctor , rationing , administrative cost excesses ) , Big Pharma ( profit mongers , blockbuster seekers ) , device and product corporations ( voracious competition , mergers and acquisitions , Wall Street suitors ) , attorneys ( litigate everything ) , hospitals ( building and tower mania , top heavy administrations and compensation frenzies ) , government ( legislate every detail ) , professional organizations ( eyes off the ball , under representation ) ? In the chaotic vacuums , certainly some abuses and dysfunctions occur in many , if not all domains . What is blocking a true health Renaissance and which culprit is most to blame ? The answer , again unequivocally , is : we all are ( shared blame ) , fundamental barriers are co located at every level and in each silo and , to an impermanent but sticky degree , attached in combinations ( but these can be peeled apart ) . Because these are all human made “ systems “ and with layered upon layered complicatifications © , they can be unlearned , co re designed , and re purposed toward contemporary needs . And then which comes first “ chicken or egg “ , nature or nurture , wave or particle – YES .
To truly AND effectively ( efficiencies alone are insufficient ) launch toward a value exponentiating HEcoSystem we need to co create a new language leading then to new thinkings , cognitions , and musings in ideal space , co designing new models and blu – emerge – prints ( not static , conventional blueprints or rigid templates ) for pro actualizing prototyping and piloting to prove – the – concepts leading to a NEXT movement of bold , abundant , optimistic Health , Wellness , and Well Being – a FLOURISHMENT . This paper will ( has already ) introduce some of this new vocabulary as tools of brain creep and stretch , transitioning toward transformational thinking . Prototypes and mathematical modelling will work in the real AND gedanken spaces to re formulate the practice of “ caring + “ . The de facto quintessential STANDARD is care and caring + ( see Maletz concept paper on topic ) . Execution of and delivery of that measurable will be customized specifically based on demographics , experience , training , judgment , resource availability , local BEST practices , and electronic records , databases , and accessible expertise . The only acceptable measure of success is VALUE AND Continual Improvement , herein , newly defined as :
VALUE = Quality / Cost x Lifetime of the Caree
Short term quick fixes and improvement blips and Hawthorne micro steps are not defined as “ true “ successes by this definition . Health and Wellness and Well Being must become a WELLBEINGULARITY © : the totipotential combining of BEST practice , thinking , execution , and ALL tools and skill sets toward a future of planetary health , healthfulness , healing , and cure of all dys – eases and dys – functions long term and as a future legacy and launch platform for more learning and improvements .
KNOWN KNOWNS
FIRST : Prevention is much more cost effective than treatment , typically a late intervention , or crisis management .
SECOND : As longevity increases , multisystem chronic disorders take their toll – hypertension , diabetes , stroke , musculoskeletal “ degeneration “ and infirmities , organ and organelle pathophysiologies and imbalances – and with these physical deficiencies and insufficiencies come decreased life enjoyment and productivity . “ Management “ and coordination of subsystem care consumes major portions of “ healthcare “ dollars .
THIRD : Social and personal preferential determinants of individual health may dictate up to 80% of measured health benefit – the essential total of which is now outside the “ control “ parameters of our current non system ( See FWM The Terroir of Health © ) .
FOURTH : Death and dying are viewed as failure . Rather , death / dying is a natural and anticipated , normal and predictable outcome of lives well lived and memories of the good , the true , and the beautiful with attendant lessons learned and stories and anecdotes to be memorialized .
FIFTH : Cure , precision diagnoses , AND prevention are much more desired and effective , than control, maintenance , or palliation and endless prolongation. The status quo is no quo at all .
SIXTH : True healthcare is Big Data writ large and growing exponentially . This must be translated into Big Intelligence . ALL points of data must be interoperable , actionable , linked , constantly updated and refined , searchable , systematized , and available to caror / caree at each and every point of care – no exceptions .
SEVENTH : New Species © must be co architected to populate the new models : PreHospitalists , ParticiPatients , PreHabilitationists , ProLiving Navigators , Information Right Speakers and Translators – to name a few .
HOSPITALS TODAY
Hospitallers , hospitality , places of rest and rejuvenation on a journey date back to the
Crusades and have a history long before science and anything resembling a scientific method or an Enlightenment were added . A cool cloth and a warm blanket , a bed and a meal were soothing and comforting . Today ‘s hospitals , depending on the country and locale , co locate technologic wizardry and various levels of expertise / training primarily for intervention when sickness supervenes . Some are waystations for mass vaccination and screenings but usually they are buildings for :
-Emergency / crisis management
-Illness / disease intervention
-Vital sign and pathophysiologic and metabolic re balancing
-Symptom abatement and amelioration
-Advanced diagnostic and testing sources
-Major surgical corrections , ablations , amputations , and organ repairs and
enhancements
– Intensive care and resuscitation in single and multi system organ failure
-Full court press death prolongation and preparation
-Places of solace and social networking for all abuses , excesses , overdoses , reckless
behavior residuals , mental lapses and psychotic breaks , and houselessness ©
In the past century we have no excuses not to celebrate and acknowledge the triumphant discoveries and curational pathways that have been initiated and compiled – from the Curie ‘s /Roentgen ‘s x rays onto CAT / MRI / PET / DTI – radionuclide scans to antibiotics to mapping the genome and epigenome . The process of 3D printing , nano technologies , remote telemedicine and monitoring , robotic and minimally invasive surgeries , molecular and regenerative biology , genomics , metabolomics , proteomics , and microbiomics await fulfillment , application and further development . Add to this a deeper understanding and proof – of – concept in the alternative , complementary , Eastern traditions , and nutriceutical and nutrition sciences and the totipotential for global health and wellness is within reach , even in conventional hospitals .
“ Pipedreams “ you may say . “ Impossible wish list “ you may affirm . “ Who will pay for the gargantuan coordination task and herculean endeavor “ ? – is an appropriate question given all the published materials on accelerating cost curves and unsustainability . First , inclusion is a proposed budget – I have located $5. 8186 TRILLION per year globally for our consideration and re purposing ( see addendum ) . Therefore , even if I am off by a few billion or even tens of billions , there is money to utilize NOW. AND more than enough . Do , secondly , we have the will and are there enough Atlases to flex to lift the globe toward health – my answer is absolutely YES – if done together and with BEST leverage . My other philosophical inclination in this crucial arena is that to effect positive change ( nudgings AND more radical R – Evolutions ) we must , based on a well communicated literature of cognitive linguistics and psychology of mind framing , co create new model consilience and novel language toward NEXT spirals of growth and development on the upending and unending maturation continuum – all BEST s , enginuity , tools , resources , norms , mores , and imaginings – ALL – are applied to this convergence , this paradigm springboard launching a bold , abundant , optimistic , positive , and always looking forward flourishing , a Health EMERGENCE .
HEALTHSPITAL 6.0 + Proposal Update 2016
In the annual meeting of the World Future Society a theme was “ WHAT IF “ . My initial writing described 5 “ drivers “ of the proposed design . Subsequent revisions borrowed from the burgeoning EMERGENCE literature and HEALTHspital was reconfigured as a PLATFORM – not THE FINAL or END point – and onto that platform of health and wellness was constructed 5 pillars . These will be explained briefly here .
PILLAR # 1 A HILL OF RIGHTS
WHAT IF in our re visioning we got every step , every situation RIGHT . The RIGHT patient : so much more than right identification and right site for surgery – the fully prepared patient , ready and optimized for any encounter . The RIGHT provider : right training, background , and experience , right skill set for that right patient’s needs and expectations every time . RIGHT site for care / RIGHT setting – could be home , office , sports field , medical space , or present hospital , pharmacy , school , walk in minute clinics . RIGHT diagnostics , testing , analytics , and imaging . RIGHT price point – amount of testing and resultant care appropriate to the presentation . RIGHT differential diagnoses preliminarily with inclusion of ALL possibilities for care and intervening – no missed opportunities to be RIGHT . The right begins with all the RIGHT questions and all the implications and potential applications for care / for caring brought by each caree . RIGHT data can then be correctly entered into local databases , crosschecked by interested ParticiPatients at their respective “ medical home “ for accuracy then added to larger population databases with detailed demographics to further population studies and with the potential for deeper pattern constructions – goals for subpopulation predictive modelling . These are described as “ hills “ , not mountains , as these types of data handling and mining are far more manageable and accessible given ever improving artificial intelligence algorithms . RIGHT information becomes RIGHT intelligence which then frames NEXT questions and identifies potent new research topics . This pillar produces a feedforward loop of learning and iterative improvement .
Get it RIGHT and then execute it RIGHT the first time and every time is the new norm . Have the outcome stay RIGHT for the patient ’s lifetime – correct AND RIGHT . None of this pillar’s principles requires a substantive cultural leap for current carors . Virtually all practitioners I know , and have the daily privilege to work beside , in this current healthcare space , even when stress , frustrated , burnt out , or demoralized on any given day , are consummate professionals with “ doing RIGHT “ for fellow humans encoded in their DNA and hardwired into their chromatin , epigenomes , and neural pathways . In the face of all extraneous pressures and burdens of our non systems , the oaths , abiding inspirations , and original aspirations will be easily rejuvenated .
PILLAR # 2 WFA / OVER – / UNDER -TREATMENT AMOUNTS / DUPLICATIONS
Again exemplars for this foundational support and a vibrant literature exist already – LEAN , TPS , and variations specific to this topic . I understand “ bare bones “ and squeezing every last drop of efficiency out . But this pillar is so much more demanding than a simplified economic model generated by our bookkeepers , econs , and quants . This paradigm must exist at the point of care – each and every time . I suspect there is some outright , intentional fraud – carors purposefully trying to work the non system and the loopholes between the complicatifications . But if we have allowed flaws in the fabric of delivery and loopholes and unreasoned gaps and vacuums to exist , advantage will be taken by these very intelligent people , advertently or inadvertently . We get what we failed to prevent systemically . Sharon Brownlee’s focused book , PCO ‘s ( Patient Centered Orthopaedics ) group , and the Lown Institute have done yeoman’s work on overtreatment . But undertreatment requiring callbacks and re works , more visits and new diagnostic cycles , adding enormous costs and hand offs thwarting a true system ‘ s view . My start in the effort in 2010 was fueled by the Magna Carta of papers – Robert Kelley ‘s documentation for Thomson Reuters of $700 BILLION per annum in the US alone that is wasted , needlessly and unproductively . Elimination of this available surplus ( ⅓ of current US spending ) would instantly bring the US in line with many other developed nations who spend reportedly less and deliver better outcomes , consistently and repeatedly . The emphasis , as previously stated , must be on effectiveness which is so much broader and interesting than mere “ efficiency “ ever connotes .
PILLAR # 3 COORDINATED / INTEGRATED CARE
Think of the nested sub- and ecosystems in the human organism : gastrointestinal / digestive , reproductive , renal / urologic , cardiac , vascular , nervous / neurologic , musculoskeletal / rheumatologic , dermatologic , special sensory , endocrine / metabolic , pulmonary / respiratory , mental , microbiomic / commensal . As we use our “ Organism “ repeatedly , exposing it to myriad internal and external agents and forces and age and stress it , dys – eases , dys – functions , and dys – orders occur sometimes repetitively , cumulatively , or both . We know and categorize the single and some interactive pauci – and multi – system diseases and syndromes . My favorite example from my own practice was a patient with 7 nested systems involved . She was taking 28 prescribed daily medications ( excluding vitamins , supplements , and over – the – counter self medications ) . She was being actively seen by 11 different doctors , sub – and super – specialists . There is an obvious spectrum of disease and treatment , providers and associated monitoring required . The EHR has been touted as THE panacea . Big Data and the avalanche of real time patient specific data will make care connect . Providers will be enabled to coordinate and integrate care . The “ Quantified Self “ is a movement gaining traction . Not so fast ! Multiple proprietary EHR s and vendors with protected intellectual property and trademarking laws and privacy strictures prevent interoperability and true interconnectivity in records and record keeping . Ignorance is NOT bliss , but neither is a tsunami / avalanche of non sensemaking raw data . Also , is the RIGHT personalized data being recorded and accumulated . Lawrence Weed MD , an early and persistent pioneer has given us SOAP and POMR , moving on to Knowledge Coupling software . IBM and Watson have teamed with the Cleveland Clinic and its Lerner School of Medicine to inaugurate new interactive methods for bringing the world’s medical literature to the doctor – patient , caror – caree relationship , co – and inter – relating best current information with highly personal fact – finding interview and physical examination skills .
When then combined with integrated laboratory and imaging studies , so refined by such highly specific database collection , assessments and treatments can be specific and customized . Yes , personalized , precision medicine . And then subsequent encounters get better and better with each iterative learning cycle.
When local intervention points are restructured , the usable , truly functional , interoperable EHR then empowers a truer “ Medical Home “ actualization – for “ Home is where ( ever ) the “ CHART is . “ Dynamic Funnelization “ © allows “ universal capture “ of all potential “ ParticiPatients “ who then integrate into global “ universal caring + “ . A local ——–> global culture of caring + is born . The dynamic funnelization is an iterative , closed looping , flow diagram gathering ALL of the patients in a community population , person by person , then patient by patient , into an ever enriching and ennobling database . Evidence based medicine becomes Best Evidence Now (BEN ) medicine applied , then becoming Best Intelligence Next (BIN ) , and then ultimately leading onward to Universalizable Best Practices ( UBP ) . These also with new research and population experience can platform build toward planetary Health quality and improved Wellness for all . Thus , Private——–> Personalized ————> Public————> Population ———–> Planetary Health and fulfillment , productivity and Well Being – A WELLBEINGULARITY © . Individuals / elements become SubSystems ; SubSystems become micro – systems ; micro – system integration builds macro – systems ; nested ecosystems expand toward a HEcoSystem and bold new horizons AND novel co created realities .
PILLAR #4 DEATH AND DYING
We got badly off track and perturbingly off course with this topic . Death panels , Dr Jack Kevorkian , and “ rationing “ of sickness care in death preparation anecdotally caught our attention. But a quiet R – Evolution has begun . Heroes and heroines like Dr Ira Byock and author Katy Butler ( KNOCKING ON HEAVEN’S DOOR : The Path to a Better Way of Death ) have moved the needle toward true north with humane discussions of care and caring as life ‘s “ end “ approaches – inevitably and naturally . We get wrapped up and embroiled in ethical dilemmas – “ When does life begin “? and “ What constitutes death “? Is it the union of sperm and egg ( full potentiality ) or the ability to sustain vital functions outside the uterus ? Is the end when a heartbeat flatlines or brain wave EEG activity goes to zero ? We are actually quite fragile and vulnerable in between our birth date and demise certificate . How long can a human being survive without food / without water / in the raw elements without shelter , heat , air conditioning ? How long could a college student remain in school without parental checkbooks and bank loans and scholarship subsidies? How many would be without shelter if not for mortgages and long credit extensions ? Life and its living are TEAM SPORTS . We are all co ParticiPatients eventually . Birthing is highly intimate and, more and more , customizable . And while taxes may be modified and even evaded , death , to no one’s surprise , is for sure , a certainty , natural . Cells die and are replaced and recycled during the entire hyphen / DASH between birthdate and death date , our tombstone enshrined memorialization of our existence . But death is NOT an end . Lives well or poorly lived are teaching/ learning moments to be treasured , revered , precious . We should treat ALL alive , living , sentient beings with dignity , awe . This is the hierophany , the spirituality that metascends © formal religions , mores , norms , and cultural traditions.
We spend an enormous amount to “ keep “ patients , family , neighbors , “alive “ , often when all know , even the patient , that this will only fruitlessly , futilely prolong “ life “ often in a hospital , intensive care bed . We speak of “ quality of life “ . Dialogue could start much earlier – “ describe in your words your BEST death “ . “ How do you wish to be remembered , memorialized “? “What legacy and life points highlight your story “ ? Instead of the flashes of photographs in funeral parlors and graveside testimonials , quickly forgotten , the “ patient “ could write the narrative , co produce their notable and favorite moments and turning points , co create and co design remembrances , videos , storyboards , and essays . The Hospice approach and family care giver training could be coached – many “ terminal “ patients prefer to spend as much time at home , in comfort , surrounded by what they built , the familiar. Death is natural – it should be treated as such . Personalized medicine and preferential , culture attuned and sensitive traditions must be applied diligently to this domain . Death is not THE END , but a baton for future generations and a lasting legacy for NEXT s .
The “ death panels “ become “ family panels “ with a patient , caring epicenter . “ Rationing “ becomes rational . “ Funeral “ homes become “ celebratory community points of light and remembrance “. “ Departed “ becomes wisdom “ imparted”. The individual is returned after “ their time “ to the cosmological whole , never forgotten , always treasured , forever missed but remembered .
Life as legacy and Death as baton – for all – forever . Again , simpler , but not too simple for such a complex topic. BUT , by mind spaciousness and language change, this new thinking could make a re investible dent in the 80% of the Medicare budget expended in the last 6 months of life – futile becomes fertile , senseless becomes sensitive and sense making , “ death be not proud “ becomes “ proud to have lived , AND DIED ” , well !
PILLAR # 5 THE NOVEL – THE EXCITING – THE PRE s PRO s RE s CO s
PRE:
-Pre Emptive -Pre Dict
-Pre Vention -Pre Ference
-Pre Monitory -Pre Pare
PRO:
-Pro Active /Pro Act -Pro Gnosticate
-Pro Mote -Pro Pensity
-Pro Tection -Pro Spective
RE:
-Re Generative -Re Patriate
-Re Juvenate -Re Habilitate
-Re Store -Re Populate
CO :
-Co Design -Co Operative
-Co Create -Co Nnect
-Co llaborate -Co Mmunity
We have gained much from our Scientific Method. Evidence based medicine and surgical protocols have produced massive improvements in care toward cure . But individuals spend an uncoordinated “ fortune “ on products and methodologies marketed and hawked without the rigors applied to more traditional measurables and deliverables .
Nutriceuticals , supplements , alternatives , complementarities abound . Naturopathy , chiropractic , and osteopathy have long and rich traditions and highly trained practitioners. Who can “ play “ in the local HEALTHspitals and the larger HEcoSystem? Everyone , inclusively . Welcome ! BUT THE STANDARD IS CARE . Health and Well Being are the outcomes – for every specialty in this new Healthspace . Proof – of – concept and patient granularities must adhere toward cost effectiveness of that care for every true health outcome achieved – and be able to stand up to scientific scrutiny – validated and falsifiable – therefore , provable . Payors must also open their minds and checkbooks to attribute improved health and prevention to premium reduction and benefit re alignments for all dedicated co ParticiPatients . Remember this is a true ecosystem. This will never again be standard insurance modelled , zero sum game . This ecosystemic goal is win – win – win ……………..+ This is to be democratized , equitable , commoditized , collective , co operative , community based and facilitated , patient centric , UNIVERSAL CARE +. This can be accomplished in toto – as a Holarchy and NOW . Many of the pieces and parts already exist , my so – called MOM s and POP s. Pieces that fit this model can be integrated seamlessly and with immediacy . Pieces than can be modified should be – to fit . Discard the rest . Then co create and co design prospectively anything missing to fill out the needed totality , Wholistic Healthcare .
THOSE ARE THE 5 PILLARS
While I am a futurist , optimist , positivist , and neosynthetist , I believe I am also a realist . The following broad categories represent roadblocks , hurdles hills , mountains , and barriers in the Healthscape :
-LEGAL
-FISCAL / FINANCIAL
-POLITICAL / LEGISLATIVE
-EDUCATIONAL / TRAINING
-CORPORATE
-CONVENTION / TRADITION / CULTURAL
LEGAL
Many legal parameters will require re evaluation and modification. A major example will be in the area of information access , especially as data becomes more accessible , interoperable , fungible , analyzed for whole populations , and granular . To be useful at points of care , it must be available and seamless just like balance data and demographics on a credit card magnetic strip are now . Privacy is paramount to consider , of course . But new laws regarding non – discrimination when applying the analyzed , de identified population intelligence will be critical , not only for genetic information . Everything in cyberspace can be hacked , and all protections can be thwarted . Health and Wellness data , genetic propensities , family and social history , past history must always be directed and used for caring+ , to care . It must NEVER be misapplied to marginalize , segregate , de – humanize , prejudice , or discriminate against individuals or groups .
HIPAA will likewise require major overhaul . Anti – “ dumping “ requirements will need allowances for re triaging and re directing patients to RIGHT practitioners and RIGHT points of care provision , in timely and appropriate manner . I have personally questioned many of my patients about their willingness to allow me to determine to whom information will be needed in their care plan , care pathways . I have yet to receive a single “ No” , after literally hundreds of such permission requests . As we have learned from hundreds of billions of social media posts and blogs , people want their stories told , usually appropriately . To move from public to planetary health , information —————> intelligence ————-> wisdom IS the highway .
POLITICAL / LEGISLATIVE / LEADERSHIP
Is health and its care Democratic / Republican / Independent / Green ? Is this arena Conservative / Liberal ? Should it be characterized by democracy , communistic , or socialistic principles? Are we speaking to political agendas whether transparent or hidden ? My unequivocal answer is YES – all could be and should be considered because “ Health “ as expanded in this model is METAPARTISAN © , and is , therefore , a metascendent , phenomenologic emergence . “ HEALTHspital 6.0 + “ is a proposed model to be included in this overarching and bold undertaking I call “ Metapartisan Mars-shots and Stars-shots “ ( not Moonshot – we have already successfully accomplished that ) . Diversity in inclusion and inclusivity of all novel applications are eagerly sought to build upon these pillars and co create even more parallel constructive spin offs and spin ups. Does this require political will and co llaborative democratic and invested participatory leadership and championship ? YES AND NO .
Leadership , conventionally defined , is hierarchical , top – down , and the fruits of its profitability often siphoned to other domains of political promise and favoritism ( pork ) . Here defined , leadership is more leaderless , participatory , bottom spreading , like an autonomous colony of expansile self organization . But this is a principled algorithm based on contribution ( see CONTRIBUTALISM ) and , always , CARE + that ennobles this Mars-shot / Star-shot . The real question is : Can we muster the universal polis , political global will and willpower , to make Health and Wellness a priority in our Global Commons ? The answer is : We must !
FINANCIAL / FISCAL
As directed in Appendix A , there is copious money to be re directed and re purposed for investment in Health and healthfulness. Why should any ONE be energized to push for this re investment ? We will all – payor and provider , caror and caree , CEO and indigent , wealthy and houseless – ALL – at one point be dys – eased , a patient , and our ultimate destination is terminal . No one is excluded or will escape untouched . Of course , fiscal data sheets , measurables and intangibles , all determinants as well as proxies for health must be re conceptualized . Also key is that transparent bookkeeping must be open so that clarity of investment and re investment is sharp and crystal to all . If , for instance , Health and Wellness outcomes yield and generate decreased intervention expenditures in a given community , active participatients should be rewarded with premium rebates and a proportion of community wide savings re invested into those same communities for bike paths , green plantings , free seminars and health education , FitBits and real time monitoring for all , screenings , nutritious food co ops , and this list is endless . Healthy behaviors and attitudes are norms – normalized to every activity of thriving life – a sustainable “ thrivitality “ © . Folks who persist in smoking , drinking excessively , eating monumentally , failing to comply and adhere to recommendations and proscriptions , continuing to ignore warnings , and who call out “ sick “ , behave unsafely and recklessly will be nudged with higher premiums , co pays , and increasing divergence from those more happy , more productive , more fulfilled neighbors – in a free society all have their choice and choices . But the default – the path of least resistance – is Health . Their opt outs must be selected thoughtfully , for the negative reverberations will be significant . To diverge from this new norm is more costly , more negative , more inhumane to those expressing and selecting this preference . And should be .
EDUCATION / TRAINING
Learning in medicine / surgery is lifelong – CME – and should be expanded as such to all domains . Abraham Flexner was our ICONOCLAST as his biographer proclaims , but his model as synthesized is over 100 years old – an obsolete , anachronistic , dino – soured entity given our Information – Technologic – Interconnected new world . Why does organic chemistry , freshman calculus , or 4.0 GPA constitute our best , make – or – break crucible for practice ? A Google search and ask SIRI place answers at our screen fingertips . Curricula and textbooks are obsolete , virtually at printing . HEALTHspital librarians become the new navigators for providers and participatients alike – vetting BEST available research studies and evidence for questions of the moment – combining international expertise to local applicability raising the care bar instantaneously whenever and wherever breakthroughs and breakwiths occur . HEALTHspital nutritionists are also mission critical in community outreach to convert “ food deserts “ into “ nutrition oases© “ , conducting home and community garden training , food selection and cooking classes , and illustrating appropriate balancing with micronutrient attention . BEST research , BEST studies , and BEST evidence translate and transfer to the bedside , office – side , or home – side wherever CARE is needed or prevention opportunities abide . Information and its infinite fungibility interconnect , internetwork with the living HEcoSystem , moving and flowing in to treatments and then out to preventions . Outcomes are openly communicated and all “ boats “ rise . Better yet , the aggregation and analytical robustness permit planetary ranging studies , fully powered by adequate sampling size , yielding more granular questions for deeper and more expanding research curiosity . CME becomes CUH : Continuous Universal H – education for all curious and interested in exploring Health and Wellness even further . Education , as re framed , truly leads us out ( L . e ducere ) from our present paradigms .
CORPORATIONS / PARTNERSHIP
“ Conflict of interest “ – an interesting term . Also “ influence “ . It is the opinion of some that a company funded office luncheon or a representative supplied logo pen will swing a practitioner to utilize a pharmaceutical or device preferentially . While there are myriad examples of abuse and colossal misfeasance still requiring oversight beyond our present puny attempts at “ radical transparency “ and “ podium disclosures “ , let us never lose sight of the massive value supplied by true corporate partners in the health insurance , medical supply and services , Big and Small Pharma , and device manufacturing domains . As we re think and re vision the Commons and co design the HEcosystem these are critical keystone and rivet “ species “ : valued , value adding , and valuenabling . Their R AND D must be integrated with problems to be solved . Research questions must be aligned with funded research. Underfunded and unfunded mandates must be replaced by appropriately funded , programmatic , internetworked proofs and pragmatics . In this space pure academicians must be respected , but even more respected will be those pragmademicians © who translate pure bench science into Health and Wellness deliverables . “ Conflicts of interest “ must become “ Confluence of interests “ in the H – Commons . Recall always “ Caring is the Standard “. Corporate profits and sustainability in the new H – Space should be more transparent , re invested , and reasonable , not egregiously excessive to the few – and then distributed globally – to be determined and co llaboratively defined , not in silos and boardrooms behind closed doors , but interdependently . Co op boards could serve as models in the new H – Economy .
COME TOGETHER
Mechanistically how can we actualize and realitize this proposed concept . I personally have worked traditionally and conventionally since my MD degree was bestowed in 1978 – private hospitals , free hospitals , “ children’s “ hospitals , burn centers , military hospitals , State mental hospitals , University hospitals , and , most recently , a Hospital regional “ system ” . I have studied and reviewed international so called “ systems” , funded care , integrated , and socialized models . When all is said , there is no universal , all inclusive HEcoSystem – YET .
FIRST , we are all patients – therefore , with skin and other organs in this game , this space .
SECOND , there is much work to be done to reach planetary Health , Wellness , Well Being – a GLOBAL WELLBEINGULARITY .
THIRD , most current “ care “ is provided locally , person to person , community by community .
FOURTH , there is ample capital available , if re purposed .
FIFTH , ALL our models – Hospital , point of care , training/ education , delivery , funding , measurements , and oversight – are obsolete , archaic , anachronistic , antiquated , fragmented , siloed , evolutionary , incremental , partial , short term , unsustainable , and value compromising – a patchwork / mosaic / tapestry – at best .
SIXTH , the call is to utilize our present BEST s in art , craft , guild , science , technology , spirituality , and pertinent , relevant , and co designed combinatorics toward novel models of integration and value exponentiation – NEVER accepting status quo or regression but only humane “ caring “ with e – quality , effectiveness , and evaluations built in for BETTER BEST s to come .
Community HEALTHspitals require no investment in more bricks and mortar , aluminum and glass testaments to philanthropy . They are a simpler gedanken experiment with major impact when taken to scale . A HEALTHspital can arise by any insightful CEO AND Board by standard top – down directives and mapping . One year of prior data and one year of post implementation data will establish singular proof – of – concept after careful analysis of Community impact . OR individual pillars can be mathematically modelled and analytics and cost accounting applied to pre determine partial micro systemic impacts . OR an “ adventure contributionist “ with interest in this “ Mars-shot / Star-shot “ , this space , could fund a prototype / pilot . OR a self organizing community co – operative could envision a local hospital ————–> HEALTHspital conversion along the model of successful food – farm co operatives in existence .
My ultimate goal , hope , never ending aspiration is to co create , co design, and co llaboratively begin a R – Evolution , a Metascendence , taking us to new platforms of re visioniong HOPE , HEALTH , HEALING , HEALTHY , HEALTHFULNESS , WELLNESS , WELL BEING , AND CARING beyond the present moment toward a true HEcoSystemic COMMON WELL TH for the globe – GlobalWELLth © . The toolkits , skill sets , technologies , and minds already exist . A novel model is needed and proposed . Who is in ? Who wants to join ? Failure is an option . Band – aids and salves , poultices and pills , ointments and exercises , are all available . But WE are better together than these . And evolution has no END .
Let ‘s GO / Let ‘s DO this NOW !
Thank You
Looking Forward , Always Further ( LFAF ),
Frank W Maletz MD FACS
- Published in News
If only hospitals were HEALTHspitals
Frank W Maletz MD FACS
Monday 16 March 2020
12 MacKinnon Place
East Lyme
( 860 ) 912 9496
Connecticut 06333 – 1533
USA
Co Founder HEALTHspital Foundation CT
FROM :
Frank W Maletz MD FACS
Pamela A Maletz RN
( 860 ) 912 9493
Honghui Feng MD
fenghonghui@yahoo.com
( 860 ) 514 2873
Saihuan Zeng RN MSN
( 860 ) 885 9888
TO WHOM :
SOME FACTS and they are undisputed :
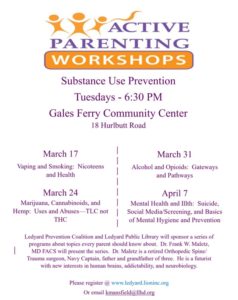
✱COVID 19 virus epicentered first in Wuhan province China and now in Lombardy region Italy is a pandemic ( WHO ) .
✱Its spread has been rapid and overwhelming in hotspots .
✱It is more virulent , morbid in selected , vulnerable populations , and with varying but more lethality than influenza viruses .
✱Roche , last Friday , received FDA approval to mass produce its testing kit ( up to now in the US , approximately 15,000 people have been tested – 400,000 will be available as soon as this week with ramped up production of 1.5 million tests per month thereafter ) – we will then begin to know what , up to now , we have not known definitely .
✱No vaccine or antiviral cocktail is curative – YET .
✱Experience has taught us isolation and social distancing protocols – with sanitation / hygiene/ precautionary principles .
✱Healthcare workers / providers must be protected , nourished , rested , and safe in order to function optimally at the front lines .
✱Viruses are NOT independent “ life forms “ – they are infecting agents with vectors ( surfaces , fomites , contact , transmission routes , carriers ) and hosts ( “ the infected “ , animals , humans ) . Viruses mutate much faster than the pace of human immune accommodations and MUCH , MUCH faster than mass socio – cultural behaviors and “ control mechanisms !
The President / VP / NIH / CDC-P / FDA / and academic and private foundations and independent expertise made pronouncements at 1530 today / updates / recommendations . This is emerging , unfolding , morphing , and mobilization with momentum is demonstrable .
In independent conversations today , an additional resource is available in SE CT ! Dr Honghui Feng and his wife Saihuan Zeng have been in direct communication with friends and family in Wuhan . There are also a number of their colleagues , Pfizer research scientists in our area with similar direct knowledge of what lessons / direct experiences have been encountered / learned in China during the past four months .
In addition HEALTHspital Foundation CT has joined with the Feng – Zeng team to propose that a database / reservoir of retired nurses , APRN s , physicians , physician assistants , and community healthcare workers and caregivers be assembled ASAP to FIRST locate those able to assist patients , clinics , testing centers , and hospitals if numbers climb AND SECOND to be provided training from BEST / current / authoritative sources NOW . A regional effort is pro active and pre emptive to integrate knowledgeable capacity to internetwork with existing institutions who may , in the near future , become overwhelmed with the actual infected or the presenting sick whose differential diagnosis includes COVID 19 .
We are part of a Community poised to help . Integrate , consolidate , coordinate , and educate us – then deploy us to augment the troops now doing front line duty .
SUGGESTIONS / OFFERS :
☯Hygiene / Surface fomite mitigation
-Contact precautions – anything touched : door handles , steering wheels , entry glass windows in establishments , food counters – cleansed after each contact ( soap and water , Purell or similar , hypochlorite / bleach or similar )
☯Eliminate hand shake , hand fist bumps , hugs , and ELBOW touch ( the olecranon is 3 – 4 INCHES from the elbow crease into which we have been instructing people to cough , sneeze , hack , expectorate , hocker – best approach is social distancing – if must touch another human , suggest facing in opposite directions and touching the heels of shoes .
☯The panic and herd mentality / hysteria in populations makes no sense : for example , why has there been a frantic run ( with , by the way , crowds of people in one place ) on red meat , frozen foods , acetaminophen ( fever reducers to eliminate health providers one clinical sign of possible infection – a fever ) , toilet paper ( this virus is NOT GI , diarrhea producing ) , milk and dairy products ( these are inflammatory in themselves ) . We could understand if there had been runs on Vitamin C and other immune boosting nutriceuticals , fresh vegetables and fruits , and bags for proper disposal of contaminated waste materials like tissues , gloves , and face masks . Social distancing is a given – individual hygiene and immune integrity is not being sufficiently communicated to the masses .
☯The CDC-P website is robust and currently updated everyday – COMMUNICATIONS are key to success – local hospitals should be the coordinating center / node for translating “ real time “ , “ at the point of care “ information and BEST intelligence to the local community – social media outlets should THEN take this intelligence and transmit it – NOT THE OTHER WAY AROUND – which creates mass hysteria and reactivity – there is “ wisdom in crowds “ which should not be ignored BUT it should be “ real “ wisdom
☯Lessons have been learned in mass casualty , climate catastrophes , and infectious outbreaks , epidemics , and pandemics in the past – these are random , cataclysmic social disruptors – we will face more – full appreciation and knowledge , solutions and cures will be unfolding as experience grows – therefore , accommodations must be made as wisdom progresses
-first awareness of problem existing ——–> dissemination of actionable , pragmatic , sensible information ( COMMUNICATION channels )
-reasoned responses based on BEST intelligence with controls acknowledging levels of medical illiteracy in the general population – in this situation , the virus has mutated to control the vector and host – hosts need to outsmart the viral mechanisms and be implemented expeditiously to counter spread and pandemia
-potential providers of care must be identified , trained on BEST practices , collated , coordinated , and centrally deployable and deployed to furnish expertise and personpower to support frontline “ troops “ – these reinforcements are then available to backfill and fill in for the initial , primary team for them to rest , replenish , and re engage
☯This experience with COVID 19 will also be a learning experience in vivo as we progress . It should be treated as such . BEST practices will emerge . The initial chaos and uncertainty , ambiguity and turbulence will be managed . Immunity AND community will emerge intact . The virus will be vaccinatable as we did with HIV . Our goal is restoration of Health on a planetary scale . We can do this !!! It must be NOW and it must be integrated and it must be ALL IN .
Thank you !
Contact information is willingly provided – call upon us !
- Published in News
White Platform: What If
WHITE PLATFORM : “WHAT IF…” AND I NEED EXPERTISE
Medicare, Managed Care, Clinton Care, Obamacare, Hospital Care, Home Care many terms have been applied to care and caring. Our “system” of care has many references in myriad articles and journals. Health and wellness, it is my contention, is a COMMONS, like fresh air and clean water. There is much to celebrate in the healthcare space and many “miracles “to memorialize. But there should be no argument that at the community level and, at best, regional micro and sub system levels there is presently NO true, integrated, interconnected, all encompassing ecosystem of health and wellness anywhere in the world to model as an exemplar YET. Hospitals and clinic hospital integrated microsystems provide sickness evaluation and amelioration, symptom abatement, death delay and dying prolongation, homeostatic rebalancing, and repair and rejuvenation of pathophysiologic aberrancies, anomaly diagnostics with increasing detail sophistication and COST for an aging population in many geographic locales. Antibiotics and chemotherapies augment, enhance, and often cure ailments, allay pain, mollify and mitigate damage. The space has yet to experience the full benefit and panoply of genomics, proteomics, metabolomics, and microbiomic manipulations. Robotics, 3 D printing, and synthetic biology and regenerative medicine will continue the incremental, evolutionary, scientific methodological progress in all fields, sub domains, and siloed disciplines.
Yet the presses roil and articles abound with barriers written by naysayers and skeptics. The cost curve is unsustainable. Medicaid will sink state budgets. Medicare will be bankrupt by 2020. Massive doctor and nurse shortages are projected and trajectories mapped. An end to Social Security is predicted. There are crises of quality and access, and chasms and gaps filled with errors and valueless redundancies. EHR s and health apps (h apps) will fuel quantified self improvements and be integrating panaceas. Precision, personalized, individuated medicine will inaugurate novel approaches BUT who will cover and reimburse for them, how will we pay for the requisite R and D and comparative effectiveness research, RCT s, and proofs of concept technologic advancements. The march of progress must be limited and rationed to effect the greatest mediocre good for the most many; cost containment and shifting, zero sum games must be instituted to “bend the cost curve”. Messes, crises, fuzziness, and chaos lurk everywhere as the gargantuan behemoth which is the healthscarespace remains untamed and out of anyone ‘s control and bounds. Resource utilization, strategic planning, and customer driven or disruptive innovation driven methodologies will save the turbulence and perturbations.
AND SO IT GOES …
The WORLD FUTURE SOCIETY 2014 Orlando, Florida annual convention theme was: “WHAT IF…” As part of that convocation the enclosed outline was offered:
WHAT IF… What if every patient occupying an inpatient hospital bed were looked at as a FAILURE OF:Care
Cure
Control
Health maintenance
Prevention
Pre emptive intervention
Diagnostic precision
Prognostication/prediction
Oversight
Education
SensingHelp
Integration
Intercommunication
Timely trending
Monitoring
Accountability
Responsibility
Healing
Dys ease amelioration
Homeostasis
Balance
This skeleton (I am an Orthopaedic Surgeon after all) suggested a framework, are visioning. Are we asking the “right questions “in the healthcare space, or, for that matter, in any areas of human endeavor and experience undergoing tsunamic change and massive information availability? When faced with turbulence, disruption, uncertainty, unpredictability, and ambiguity the RIGHT QUESTIONS are hierophanous and ennobling. And liberating. What bright minds could now be re directed and re purposed to embark upon the probing of these bold, new, insightful divergences from the present course and “inevitabilities”?
Also, WHAT IF…there were $5.64 TRILLION to dedicate to this re framing? (Enclosure and there are).
Could a straightforward question co create a paradigm launch leading pro active designers to catapult exponential organizations and microsystems toward platforms allowing even more emergence and progress? (I strongly suggest and believe we humans are that smart AND resourceful.) What cross disciplinary and combinatorial multiple pedagogies could be re purposed in the co design and co creation of NEXT + exemplars of excellence and achievement?
THINK (the WHATs):
- SOCIAL JUSTICE / SOCIAL PROGRAMS
- EDUCATION / TRAINING / SCHOOLING
- POLITICAL
- ECONOMIC / FISCAL / BANKING / INVESTING
- GOVERNANCE
- ORGANIZATIONAL / INSTITUTIONAL RESTRUCTURING
The WHEN (now on our watch), the WHERE (nowhere> NOW HERE), the WHO (us), the WHY (sense of urgency, current models are not ecosystemic many things are broken, dislocated, disjointed, fragmented, dys functional), the HOW
(multidisciplinary, combinatorics, best wisdom of best teams) Where could this begin and how to start?
The Healthcare Space and Today, for example:
THEN WHAT IF…
As providers of care make the current rituals of daily rounds (hospital rounds, team rounds, grand rounds, rounds and huddles, walk a rounds) and consider ALL visits and encounters in every “hospital” (think: house call, office, clinic, walkin, and hospital) STOP and review the FAILURE list above.
And instead of considering admission and readmission rates, patient satisfaction scorings, computer data entry and busywork, providers AND patients (caror AND caree) consider together ecosystemic ways to prevent the ADMISSION in the first place, eliminating sudden needs, many acute events requiring ambulance rides to ED s, and general crises managements.
What would this look like from an economic / planning / insurance / political perspective and how would this model and graph and compute (THIS IS WHERE I NEED THE HELP!!!)? What could the future look like and how would the trajectories be DRAMATICALLY different in the model as to
- Bed availability
- Resource management
- Utilization
- Projected future needs
- Doctor / Nurse / Extender “shortages”
- Cost and expenditure trending
- Hospital bottom lines and trending
- Planning and strategy
- Resource deployment globally
- Education / training / CE for next carors
- Global health, wellness, well being, and productivity
Finally, recall this is only a PLATFORM feel free to build on it from here.
Thank you for attention and any constructive critique!
Frank W Maletz MD FACS
Orthopaedic Surgeon
Futurist
- Published in News
Relationships
Ken Wilber ”Everyone is right“.
John Gardner “What we have before us is a glittering opportunity of unrivaled promise, which
is disguised as an insoluble problem“.
A . DOCTOR PATIENT / CAROR CAREE RELATIONSHIP
This relationship at its foundation is the quintessential interrelationship that gets many of us energetically out of bed each (and every) morning and keeps us up reading and thinking, investigating and innovating each (and every) moment into the night. Moment after moment. It is unarguably one of the three most precious, sacred, intimate, personal, intricate, and noble interactions ever conceived. The others, of course, are parent child and united couples. The “relationship”, as labeled and defined , in today’s healthcare space, is far too narrow. Certainly care and cure can be provided by a physician at a bedside in a hospital. But caring can also be rendered by a neighbor or family member using social media training tools and telehealth monitoring with nurses and advanced practice MD/DO extenders. PA s, APRN s, physical therapists, trainers, occupational on worksite specialists, nursing home volunteers should also be in the giving and contributing equation, often unpaid and always underappreciated in work force analyses and projections. And, to be equally clear, today’s hospitals are hardly ideal places for health and wellness actualization. Hospitals are good at symptom abatement, disease and sickness crises management, vital sign rebalancing, and as intensive focused facilities for death preparation and life prolongation. Here too we must broaden our horizons and fracture our constrained mindSETS and be more co creative as we address the US (and planetary/global) non system of health, wellness, and well being delivery to each and ever one of us. For no one is immune or exempt from dys-ease or, ultimately, death.
B. VOLUME
Volume, in this context, implies more, just in time, quantity, speed, velocity, numbers and similar performance metrics. There are a lot of us who now, and will, need carors, not just payors, for these ministrations: 7.3 billion on Spaceship Earth and growing. The cost spiral is unsustainable, we are repeatedly told. Bend the curve before it breaks, bankrupts us. Providers must do more services with fewer and dwindling resources. The patient must refrain from asking for the latest and greatest technological advances and assume greater and greater copays and enlarging deductibles cost sharing and shifting as premiums skyrocket. Volume and increased throughput with elaborate marketing schemata will assure improved market share and continuous cashflows. Be like Disney, and patients will gladly endure long lines and protracted queues to end in a 5 10 minute visit with a harried and distracted human staring into a pre templated computer screen while texting on an iPhone. Volume implies more and more, faster and faster, ever increasing flow. Electronic health records and Big Data analytics are tools to effect this transition. Efficiency experts and time matrix management protocols are added to our recording requirements by myriad consultants. Operating rooms must start on time, eliminate turn over time, squeeze time from hand offs and minimize breaks and lunch reliefs. Wait times in ED s and clinics must be shortened to increase the patient satisfaction scores and increase volume of services delivered. We will compensate for falling reimbursements by increasing volume and, of course, volume equates to more hospital beds filled, more services, more prescriptions, more imaging, more treatments and interventions. This generates more fees paid for more charges billed. And we wonder why, with an aging and (because of our discoveries and research) healthier and expanding population, expenditures are spiraling. !REALLY?
C. VALUE
The “new” mantra is value. We have traded “outcomes” for the old “results”. We speak of consumer driven healthcare and patients as engaged co participants despite the exponential complexity of the healthcare space. Value is often defined as quality divided by cost. Some more recent publications have modified the “equation” as quality divided by cost over a timeline. How should value be measured? How long should follow up be on the timeline? Econs, quants, MBA s, administrators, managers, academicians, and theoreticians are bright and prolific . What societal value is appropriate for a QALY: $50,000, $100,000? How should DALY s be introduced along with intangible and less concrete deliverables? What value is well being and productivity? Which social determinants of health and wellness are to be prioritized, most valued? Comparative effectiveness guidelines are developing to measure and compare our actual deliverables so as to attempt to qualify AND quantify benefits and determine what will be covered, insured, allowed. What happened to Hygeia and the customized, individualized, precision, personalized craft, art, AND science we have to offer. While, as an Orthopaedic surgeon, I am delighted that total hip and knee arthroplasty, herniated discectomy, and fusion for degenerative spondylolithesis made the effectiveness QALY cut, what about my revision Dupuytren’s contracture releases after failed collagenase treatments to allow me to continue working for another decade, or for my experimental cancer care and surveillance? How also do we bring value to the impoverished, rural, medically underliterate population groups who lack sufficient and necessary access for universal participation to the new tool kits of telehealth and quantified self monitoring wonders and health apps (h apps). And, what exactly is QUALITY? That bar for humans should be very, VERY high indeed consistent, exceeding expectations, durable, reliable, enduring, dependable, based on best evidence now (BEN), and deliverable across the entire spectrum of care by responsible, accountable carors. But not perfect. Quality, like safety, must be carefully and deliberately improved, and lessons from less optimal outcomes AND extraordinary miracles must be learned and disseminated quickly, if not immediately. But the blame game, the economic credentialing, the micromanagement, the “never” events, sentinel event reporting trails in an imperfect, very human, non system cannot, and will not, get us all to the value stream, value added, value propositions to which we aspire . And the time component is paramount. We must re vision all timelines to be patient centered, lifelong. We must increase the time for true listening to our patients vital clues are in each patient’s stories his story and her story. Interventions in the value healthcare space must be intentionally re designed to last a lifetime. But again, repairs fail, acute becomes chronic, and mechanical substitutes for biology wear out and fatigue as expected and predicted. The reality is life. A life, at present, is a chronic condition with a known but timing uncertain end point that is finite. Life is a terminal condition. Optimizing health and well being during that life, each human life, is an honor, pleasure, a profound privilege, and an ennobled greater purpose for any true caror. Thus, value is double edged and contributions to productivity and flourishing, even eudemonia, are inherent in the value the patient provider/caror caree relationship encodes.
D. RECONCILIATION
Health and wellness should be acknowledged to be a COMMONS. If you are well and happy and I am well and fulfilled, our society is well er and happier because of us both. If you, on the other hand, infect me and I become sick and need services and cannot function for a time, the gross domestic product declines and society loses a bit of productivity. Those bits and losses add up quickly. So, is it volume, or value? It is both therefore, VALUME. The answers to our perceived problems and costing conundrums must be more inclusive and next curves co created by purposeful novel designs, new paradigms catapulted and launched, not just shifted, like costs. Honor and laurels must be given to the giants on whose shoulders we stand: Bortz, Teisberg, Christensen, Millenson, Porter, Cosgrove, Lee, Kuhn, Meadows, Merry, Morrison, Watson, Crick, Venter, Flexner, Darwin, Cutler, Berwick, Sackett, Bhandari, Fleming, Pronovost, Cousins, Hippocrates, Nightingale, and so many, many others. They have tackled and masterfully addressed in thoughtful writings, solutions to parts of the gaps, lapses, and lags in the healthcare space the healthcare behemoth. Our inventors and their inventions, discoverers and their discoveries, researchers and their research, the partnerships of companies and organizations, government and NIH grant awarders, private and public foundations and think tanks all must be celebrated for the past 100 years + of cures and deeper molecular understandings, explanations, and clarifications . But the volume AND value of health preservation and well being is a humanistic interrelationship of the highest order, truly a hierophany. We must re vision our philosophy and re purpose our skill sets and tool kits accordingly. Volume and throughput are totally appropriate for the routinized, solved and solvable, straightforward healthcare needs. Minute clinics and focused factories (eg the Shouldice Hospital for inguinal hernias) with rapid diagnosis and instant availability of known end points are very satisfying and cost efficient and with high and predictable quality. Yes, they are fragmented and piecemeal and tend toward impersonal mass production, but, when merged with fungible and searchable electronic health records and integration to robust medical homes, more acceptable. TPS and lean principles have been fitted to these “assembly line” processes with Ford, Deming, Shewhart, and Codman as exemplars. Quality is actually heightened at these rights points of care. Efficiency is a term most appropriate in these routinized, commoditized realms. As more knowledge, and ultimately universal wisdom, is accumulated, guidelines, checklists, protocols, and algorithms can be developed, pruned, refined, and disseminated to h apps, to patients, and to the right licensed level provider/caregiver/intervenor/caror. “Cookbook” medicine and surgery paint by numbers, I hear rumbling in the background! Remember, great chefs write cookbooks to distribute kitchen wisdom, prevent preparation pitfalls, assure consistency, and share their refined “secret sauces” for the benefit of all, at all levels of taste and preference. This is the “chefing commons”. This, furthermore, does NOT prevent or preclude other burgeoning “chefs” from improvising, improving, experimenting, exploring, combining, or celebrating the original, the source. And, in this intimate human domain of healthcare, mechanisms must be co created that allow value exponentiation. Genomics, proteomics, metabolomics, microbiomes, and Nature/nurture and environmental co factors are applicable. This is complexity science writ large. Time must be allotted and incentivized and aligned in the true health ecosystem (h ecosystem) for the five time operated “failed back patient” in chronic pain with 28 prescriptions, 5 comorbid microsystem diseases, and 8 subspecialists opining on each subsystem. (This is a real case in my practice.) This person came for hope, help, care, mending, trending, treatment, and to have all of her issues and questions addressed. A 10 minute initial visit with high volume throughput parameters, I think not. Life goals and expectations must be aligned with deliverables from biochemistry and molecular biology to techniques and surgery. What is value to this human being? What is quality? Is cost an issue? What are priorities? Is picking up a first grandchild without pain too much to ask by her of me? Every caror has unique and wrenching anecdotes and intimate highly personal stories in memory. We all have nightmares about our mistakes and failures and failings whether personally or systemically through root cause analysis and gut twisting malpractice venues. Our inadequacies and insufficiencies weigh heavily . But we are learners, and these are teaching moments. We love our profession and calling for the continued wonders of cure and correction and rejuvenation our skills have wrought, and the gratitude earned from those helped and restored. Value, therefore, is an absolute, a must, a given, a default moving forward.
E. FINAL THOUGHTS / NEXT STEPS
Can business and medicine/surgery/care co exist? They already do. If we have a mission (and we do, and it is a noble one), there must be a margin whether in a not for profit or for profit economic structure. And, if we have positive margins, then reinvestment is possible and critical to broaden and enhance new missions thus, the TRIUMPH of the commons. Panacea AND Hygeia converge again, just as value AND volume merge. The routinized and commoditized production line templates do not necessarily have to be impersonal and cold and dehumanized, but patients must expect the tradeoffs to get the benefit of rapid access and attention, convenience, and lower charges with appropriate level of expertise. The more complicated, involved, convoluted, and difficult or, even unknown, diagnostic dilemmas and multi lemmas require our highest expertise, research commitment, time, patience, and a spacious open mind and open tool kit. Our humanistic calling demands nothing less, and our individual humanity will allow nothing less. Therefore, our new healthcare delivery models must be designed, co created, crafted with all these noble and valumed ends in mind with no barriers, excuses, qualifiers, or constraints to our thinking and ingenuity. Next generations of carors and carees will be similarly ennobled by our concerted and deliberate efforts to re vision our fragmented, dislocated, broken non system of healthcare and wellness delivery patient by patient, caror to each caree.
CAN DO!
May each of you, dear readers, have a mindspacious day/life!
Looking forward, always forward,
Frank W Maletz MD FACS
NEW EQUATION : Expanded
| VALUE = | Quality / Durability / Worth / Contribution / Positive Exponential Outcome / Output / Performance / Ingenuity |
x Lifelong / Long Timeline / Extended Follow up |
| Cost / Price / Charge / Bill / Expenditure / Reimbursement / Input / Resources |
- Published in News